When the day becomes the night and the sky becomes the sea, when the clock strikes heavy and there’s no time for tea; and in our darkest hour, before my final rhyme, she will come back home to Wonderland and turn back the hands of time.
The Cheshire Cat.
There are very good reasons why bathrooms are located at a remove from the dinner table: one should never defecate in the place where one eats. A barrister reminded me of this old adage one evening at dinner after I had bemoaned Ireland’s corrupt medico-legal system wherein plaintiffs (or more often their solicitors) pay their GPs handsomely to write medical reports for insurance claims. I’m sure my barrister friend would agree, however, that when the dining room has depreciated into the vandalised shell of an old tenement; it will inevitably become prone to unhygienic and antisocial usage.
No doubt it will surprise some to read of a GP complaining about General Practice and biting the proverbial hand that feeds. However, my position within the establishment is ‘as safe as houses’ after my criticism of Covid policy and the role many of my colleagues played during the pandemic. This led to me closing my practice in North Dublin, having resigned my appointment to the Medical Council in 2020.
I was subsequently placed under investigation for attending a public rally against lockdowns, and soon (three years later) the Medical Council is to decide upon my punishment, and that of the other doctors who failed in their duty to promote, unquestioningly, Government policy. Apparently, we were more influential and more of a danger to people than the Taoiseach or the TDs and judges in attendance at ‘Golf Gate’, ‘Party Gate’ and ‘Concert Gate’ etc.
Today I have little invested in General Practice. In truth I have come to see it as a social ill rather than an overall benefit to society. I knew it was unwell prior to Covid, I had taken up my Ministerial appointment to the Council in 2018 in the vain hope of changing it. My experience and the silence of so many colleagues during the Covid years, suggests to me that the illness may be terminal. Its pathology is genetic and runs much deeper than the financial incentive brought to bear on General Practice throughout the pandemic.
Myself and other Covid policy critics, have little left to lose, other than our licences, and a shared sense of disappointment in our profession. Realistically, I feel that disappointment could only be lifted by an unlikely paradigm shift; as such it will probably stay with us until the end. Having adhered to the Covid guidelines, yet being entirely guilty of the ‘crimes’, hopefully we will hold onto our licences and continue to be able to make a living. There are no guarantees. The establishment remains angered by dissent, and can be brutally vindictive when it wishes.
Medicine is sometimes described as something of an ego trip. I have to admit that on occasion it has become one for me, but not in the manner you might think. What I mean by ego trip is that lately, should I glance at headlines on the shelves, or overhear the radio as I push my trolley down the supermarket aisles, I find myself nodding and even chuckling quietly to myself.
The truth in respect of the Covid years remains as politically toxic as any virus. Occasionally however, it leaks into the air in flatulent forms of ‘I told you so’. I’m not alone in this mad little trip, the few doctors who spoke up against; nursing home deaths, masks, lockdowns and compulsory vaccines, also share in this little Pyrrhic victory.
We continue to be gagged, pursued by a certain cabal who pull the strings from within the medical establishment. Excess deaths, missed cancers, suicides and vaccine related injuries cannot remain concealed indefinitely. To coin a hopeful phrase from the current ascendancy ‘tiocfaidh ár lá’. Given the hitherto impossibility of their day ever coming (as it might at the next General Election); so too might we hope that ‘our day will come’.

In the Rare Auld Times
I have been practising as a GP for more than twenty years, and regardless of current trends in a more progressive parlance, I don’t mind expressing a fondness for things like community, traditions, or even the old-fashioned notion of ‘the Family Doctor’. Some things are not ‘old fashioned’ at all. That’s just a term that is applied in the pejorative, for particular motives.
In the olden-days (whenever they were), a reference to ‘years as a Doctor’, might have scooped some credibility from the idea that the longer one has practised at something, the better one performs in the role. Like poker or potty-training, practice means you are more likely to win, and less likely to ruin the carpet.
Today, with the exception of less technologically dependent skills, like piano or pottery, the longer one has practised, the more likely one is to be outdated; married to ‘old fashioned’ or ‘primitive’ methods.
Technology has become synonymous with progress towards the good. For many people, it has made the GP as redundant as the old notion of growing your own vegetables. In today’s world of instant food and information, people rarely visit the GP to dig up an ‘expert opinion’. Everybody’s got one of those – either in their head or at their fingertips. Many patients have already self-diagnosed, long before they’ve reached the waiting room. What they need is a signature, a scan, a test, a vaccine, or the usual panacea of the antibiotic. Augmentin has become a household brand-name, all too often (I am told) it is ‘the only one that works’.
It is an important and relatively recent development in medicine that there is no longer a distinction between what we ‘want’ and what we ‘need’. The distinction remains a valid one, but there are few people we can trust to make it for us. Most antibiotics prescribed in General Practice are prescribed inappropriately, and more often, solely on the basis of demand.
The internet has turned medicine into something of an amateur sport, one that everyone has a duty to participate in. I often hear people in the shops or passers-by on the pavement, applying diagnoses and medical terminology as though they were talking about cooking. Most people, with a rudimentary education, presume to know as much about a particular disease as the average GP. Often (but not always) the presumption is not too far off the mark.
The General Practitioner, despite his oxymoronic designation as a ‘specialist’, has become a somewhat self-conscious ‘jack of all trades’; anxious to avoid complaints and keep his dwindling supply of private customers happy as Larry. Being an expert on nothing, he can be challenged on almost everything, except maybe golf or football?
He does, however, remain slightly relevant to the average family as a sort of ‘medical handyman’; useful in the confirmation of a diagnosis, the issuing of prescriptions, or stamping forms. He’s not a real plumber or electrician, of course, but he can usually put you in touch with one and ‘get the ball rolling’ so to speak.
The erosion of his standing within society may have added to his insecurity. Lately he must increasingly rely upon the government to validate his existence and to mandate the attendance and the dependence of his flock.

By Trade I was a Cooper
Present company excluded, GPs are (generally speaking) not stupid people, we are at least educated, and some (among the old-fashioned ones at least) might even supplement their phone usage with an occasional book.
Many in the profession are not oblivious to the technological annexation of the lands that once belonged to the General Practitioner. Video and phone consultations are a cheaper and more accessible alternative to a waiting-room full of germs and viral pathogens. These types of consultations were becoming the ‘new-norm’, long before the current ‘new-norm’ replaced the older one.
Impending social irrelevance is a bitter pill for any professional, but we humans are a resilient lot. When plastics and Tupperware made the tinkering of the travelling community redundant, they wisely moved into tarmacadam and power tools.
Equally, General Practice must evolve as it struggles with its own increasing redundancy. During the pandemic, when the government invited GPs to an orgy of self-validation; saving the nation with a dirty cloth-mask and a syringe full of experimental vaccine; few of my colleagues asked any questions at all.
Few resisted the temptation of becoming a ‘hero without a cape’. Fewer still were impervious to the largess and financial incentive, associated with logic-defying Covid Policies. Even the then Taoiseach Dr Varadkar, cashed in on the kudos. He rejoined the Medical Register, and flew to Halting Sites to test the travelling community. What a tragedy it took a pandemic for a Taoiseach to fly to a halting site.

On the Corruption of the Youth
Lately, when I work at the out-of-hours service in Dublin, I do so in the company of a junior Doctor; a GP registrar whom I am supposed to supervise and teach for the duration of my shift. They are fortunate enough when assigned to me, as I hardly know enough to practise medicine, never mind teach it to anyone.
When I chat with these ‘newbies’ I am always surprised at the level of uncertainty they express in respect of their approaching identity as a fully qualified GP. In real terms what does that actually mean anymore? Most of them tell me they are seeking a ‘work life balance’, something very much at odds with the stubbornly persistent notion of what a family Doctor actually is, or perhaps was. A doctor who knows his patients and their families by name? Someone with a small efficient surgery in the heart of a community; a clinic where wounds are sutured, and lumps and bumps are removed or biopsied? Someone who does house calls, and stays for a cup of tea after the final palliative visit to the mum or dad who has just passed away?
Or is the modern GP a youthful, tech-savvy doctor in a hospital scrub top? Someone who works three days per week at a large office block with a shiny glass frontage? A reticent and cautious professional type, who refers the dying to the palliative care team, house calls to the out of hours service, and anything requiring intervention to the relevant ‘specialist’ at the hospital?
The former is an endangered species, confined to the fringes of rural Ireland.
The latter, the GP who works on contract at the busy clinic with the impenetrable waiting list, and the unfriendly receptionist, he or she has become the aspiration and practical or empirical reality.
Woke up one morning, looked out the window and I struggled for something to say, but you, you left me, just when I needed you most.
Randy VanWarmer
Not so long ago, my daughter interrupted some sage medical advice I was attempting to cast at her feet, by cooly stating: ‘Dad, who needs a GP when you have a smartphone?’ Her generation is an increasingly rare occurrence in the waiting room. Young adults have replaced most of what’s on offer at the GP, with a faster and cheaper consultation with Siri, Google, or Chat GPT.
Pharmacists issue medical advice, along with; contraceptives, skin care, and a host of over the counter remedies for common ills. Alcohol, Red Bull, illicit drugs, and street-Xanax are self-applied to a real epidemic, currently plaguing a generation. That hidden disease of mental illness and drug dependence is managed by parents and barely registers on the busy radar of Irish General Practice.
Young adults and teenagers have voted with their feet, unless they need a cert for school or for social welfare payments. The disengagement of young people (if they were ever engaged in the first place) is perhaps one of the sadder realities of General Practice. Arguably they are the cohort most in need of help in coping with; the porn, the drugs, the pressure, and the paradox of choice they must navigate alone, with a smartphone.
At one extreme we have the absence (or abstention) of young people, at the other extreme we have the professional neglect of elderly people within the Nursing Homes. The space between these two demographics, contains some of the abysmal failures of General Practice as it exists today and that is to say nothing of the unique needs of a diverse immigrant population, one that GP’s are neither trained nor even encouraged to understand.
What if the pharmacist could stamp forms or if patients could vouch for their own sick leave? Or if they could simply refer themselves for a routine blood test, or an appointment to see a consultant (as private patients often do); General Practice would be about as socially relevant as tits on a bull. If a couple of antibiotics were available over the counter (as they are in many countries), the meteor would impact and the dinosaurs would shuffle on towards oblivion.
Arguably there is precious little that an average GP can or will do in the community that a competent Nurse could not accomplish quickly and efficiently. Today, almost all minor surgical procedures are referred into queues at the major hospitals. In north Dublin the Out of Hours Service will neither suture a wound nor syringe an ear, which seem to be risky interventions in these litigious times. Almost everything nowadays is referred to a ‘real doctor’ at the hospital.
Ironically, the burgeoning bureaucracy of forms is not the bane of General Practice, it has become the umbilicus. A newly qualified GP can be as competent as he likes in respect of medicine yet, if he does not know how to use the practice software, to tick boxes and lodge claims for a myriad of HSE chronic-care payments, he or she is essentially unemployable.
The traditional mythology surrounding General Practice, the institution’s relationship with the HSE, all mean that like the banks, it is ‘too big to fail’. For example, the training body responsible for the production of new GPs (the ICGP) has complex ties with, and is paid by the HSE.
Like a recruiting agency, it supplies them with Doctors, who fill unattractive hospital posts around the country, as part of their ‘training’. These trainee GPs are also farmed out to provide free labour for select GPs around the country, whilst both the trainee and the ICGP are paid by the HSE. The ICGP is one of those illustrious quangos we Irish are in love with; a ‘registered charity’ with freebies for friends and financial investments as far afield as Saudi Arabia. Colleges and ‘non-profit’ medical organisations like the ICGP and the RCSI., pay no taxes, they share the spoils out in the form of benevolence, salaries and expense accounts.
The entire system of medical training in Ireland is defined by deeply embedded and legitimate forms of nepotism and corruption. Beaumont Hospital freely provides almost everything from patients and teachers to the toilet paper, for the Royal College of Surgeons. The College is a private medical school and it charges students up to €58 thousand per year in tuition for the six year course, three years of which are conducted at Beaumont Hospital. Bizarrely (or perhaps not) this private medical college is sustained by the largest ‘public’ hospital in the country.
Consultant Professors of this and that, can hardly find time to attend to surgeries or public clinics. They are often busy down the hall, at another theatre, lecturing to Saudi Princes and Emirs from Kuwait.
The RCSI (another registered charity), owns and operates a second Private Medical School in Bahrain, where it offers private medical training to Canadian and American Medical Students, for around €44 thousand per annum for the six year degree.
The Taoiseach’s leaking of contractual negotiations between the HSE and one of the rival GP organisations, is merely the tip of just one iceberg that has recently floated by. Off to melt away in warmer waters; like the long-forgotten intrigues and scandals at the IMO another quango who’s last CEO retired amid a teacup of controversy with a pension of ten million euro.
Medicine in Ireland, particularly medical training might well be described as a fermenting vat of rot. We have no swamp; the water is too putrid for any genuine forms of life, reptilian or otherwise.
The drugs don’t work, they just make you worse…
Richard Ashcroft
The vast majority of medicines consumed in Ireland are prescriptions issued by General Practitioners. The Pharmaceutical industry from the local Pharmacist to Pfizer itself, depends on GPs for those scripts. A need that is more prescient and influential than those of any particular patient cohort.
This year, circa two billion euro in Exchequer funding was paid to a few pharma companies in return for drugs covered by the medical card scheme. That sum could be more than halved if a National Formulary of prescription drugs was put up for tender each year, as is the case in other countries like New Zealand for example.
Pharmaceutical lobbying, however, discreetly maintains the status quo. In Ireland corporate lobbying will hardly be investigated by a mainstream media, dependent upon corporate payments for advertising revenues and the salaries of A-list celebrities. The general acceptance of corporate influence over the state broadcaster suggests that most Irish people think ‘lobbying’ is something that might pertain to Wimbledon or tennis.
A prescription is often the most efficient way to end a consultation, it does not cost the Doctor a thought because they do not cost him a penny. In Irish Nursing Homes most residents have an extended shopping list of pointless medications, the phenomenon is referred to as ‘polypharmacy’. Many of the frail and emaciated are taking statins, in order to keep their cholesterol down; it’s a little bit like putting famine victims on diet pills. Sleeping pills, sedatives and expensive food supplements to compensate for an unpalatable diet of gruel are the norm for many.
As a consequence of being interlaced with a political and pharmaceutical agenda, and in abeyance to a certain type of mythology associated with the family doctor; Government underwrites General Practice to the extent that it consumes as much, if not more exchequer funding, than the entire Public Hospital system. Last year it cost four billion Euro to pay for GPs and Medical Card Prescriptions, an increase of 49% since 2016.
General Practice is a little bit like a religion in that it is sustained by some established patriarchal ideals. The notion of ‘doctor knows best’ or ‘just what the doctor ordered’ etc., is possibly more embedded in post-colonial or post Catholic societies.
Following the collapse of the Church in Ireland, the GP has become something of a locum tenens, for the parish priest. His is an ‘evidenced based’ religion, one that promises a healthy life; in place of the immodest and unsubstantiated offer of an everlasting one.
Despite a paucity of practical reasons for its preservation, General Practice is nonetheless sustained by popular demand, as a kind of impractical luxury. Like paying rent for a Lamborghini when a bicycle would be overkill. It is difficult to know whether the costly underwriting is motivated by the mythology; or whether it is mandated by the institution or the many others who gorge themselves upon a Health budget that knows no limits.

Church & State
The political preservation of General Practice is accomplished in several ways. You can be as sick as you like, but you will only get paid once the GP signs the IB1 form. Ironically if you are in hospital, a hospital Doctor will give you an IB1 form that you must then bring to your GP and pay for the pleasure of his or her signature.
GPs are responsible for the care of every elderly resident within the depressing environs of the Nursing Home Sector. In Ireland a Nursing Home can neither open nor operate without the supervision of a registered GP, a supervision that is at best light-touch, but is heavily paid for.
Illness benefit, driving licences, passports, nursing homes, access to the public hospital system, to the Emergency Department etc etc., are all stamped and signed by General Practice. These are the lands that belong to a post-colonial landlord, one who operates behind the general facade of a liberated Ireland.
Pharmaceutical companies have an ever increasing need for community GPs to push an agenda of pharmaceutical dependence upon the entire population. Arguably this agenda has gone unchecked for over half a century. Pharma companies provide jobs in Ireland and advertising revenues for the mainstream media, they should never be questioned; and so the executive board of the HPRA is dominated by ex-pharma employees.
Opiate dependence is barely a scratch on the surface; antidepressants, benzodiazepines, Lyrica, statins, antibiotics and polypharmacy in the elderly are more disturbing realities. Each of them are lucrative social tragedies, rarely spoken of in public. Like excess mortality or vaccine-related injuries they are confined to the realm of ‘conspiracy’.
Learned and encouraged helplessness within Irish society in respect of basic health, fear mongering by pharma and state agencies in the guise of various ‘health promotion’ campaigns, means that there will always be the need for a Doctor in the community; one who is almost as skilled as a Nurse, but has all the power and influence of a mafia boss.
I just checked in to see what condition my condition was in.
Kenny Rogers
Thirty years ago when I began to study medicine there was this crazy notion that Doctors would ‘cure’ or ‘fight’ disease, whenever possible. That same general expectation of ‘cure’ has all but disappeared from the everyday language of modern medicine. It is no longer expected of the GP to cure, or even to attempt to do so. Long-term illness and ‘chronic management schemes’ have become the ‘ne plus ultra’.
Ironically, apart from cancer, the biggest killers in Ireland are indeed curable diseases; heart disease, type 2 Diabetes, vascular disease, obesity, depression etc. In recent years all of these conditions have evolved to be considered solely in the context of ‘chronic disease management’, associated with chronically diseased payments.
The gaping irony hardly registers. When I mention it to the trainees they return a blank confused expression, as though I were suggesting something possible and impossible at the same time. There is no space within the establishment to discuss the question as to how or why GPs have become facilitators instead of healers? This is another conversation generally confined to the realm of conspiracy.
In Ireland today illness is managed, no differently to a business, wherein profit is the bottom line. Tellingly, amid the mind-boggling array of payment types issued from the HSE to GPs, there is not a single payment or financial incentive in respect of ‘curing’ anything at all, never mind any of the curable diseases that actually kill most people.
In New Zealand, where I completed my GP training some years ago, GPs were actually paid a bonus if their prescribing of antibiotics remained below the national average. Most disease was treated (and often cured) within the community setting. In Irish General Practice ‘cure’ has become an anathema and disease has become our raison d’être.

Image Daniele Idini.
Halcyon Days
Any real or practical value that the GP brings to public health is (or was once) contingent upon the fading reality of the somewhat old-fashioned ‘Family Doctor’. That GP was (and occasionally is) part of a community of people living in close physical (as opposed to digital) proximity. People who are mutually dependent upon each other and the community, in small but positive ways. In the modern world of sprawling high-density estates, the notion of collective, integrative and supportive communities, is becoming little more than a sound-bite that estate agents use to sell houses.
There was once a time when the GP knew all or most of his patients very well. That knowledge was an essential and fundamental clinical tool, as important as the stethoscope, and impossible to replicate through any amount of technology. It was that intimate knowledge that would often determine an intervention, and whether a referral to the specialist was immediately necessary, or necessary at all.
Outside of the paperwork, most presentations in General Practice are motivated by some form of anxiety or worry. Intimate knowledge in respect of the family and the individual often allows the GP to distinguish between anxiety and pathophysiology.
Sometimes he might have got it wrong, but more often, he or she was in the right place. This lack of distinction or inability to distinguish between anxiety and physical pathology, is one of the things that annually overwhelms the health service. It is almost never discussed and is expressed regularly in the unintelligent language of a: ‘shortage of hospital beds’ and a ‘shortage of doctors’. We may not have a shortage of Doctors, rather than a genuine shortage of doctors who know their patients well, or know their patients at all.
The Doctor’s sometimes sage advice was an imperfect thing, derived from his unique knowledge of the person, from a love of learning and an understanding of science. He was also the victim and the enforcer of a particular zeitgeist and strict social paradigm; that aspect of medicine has never changed.
Although it remains a rather lucrative enterprise to have one’s HSE-income, and share it with no one; single handed practice is taxed with an unhealthy level of responsibility. No newly qualified GP would dream of setting up alone in today’s Ireland. Few, if any, single-handed practitioners could provide the type of service that people now expect. Sole practice was the first limb of the cat to vanish. The once ubiquitous ‘walk-in’ surgery once had a financial incentive, supposedly socialist medicine however is strictly by an appointment, generally for sometime next week.

Working for the Man
Presently in Ireland a couple of large corporate entities are hoovering up what remains of the small suburban practices or those rural practices with profitable lists of Medical Card holders. These companies will buy a practice and keep the principal GP on as a paid employee in order to control his Medical Card list.
For the most part, newly emerging GPs know nothing of the ‘halcyon days’, and are generally happy to start working for ‘the man’. They cannot be accused of selling their souls to the devil. In contemporary General Practice there is no place for old-fashioned things like souls, despite the overabundance of devils.
Such corporations pay 12.5% in corporation tax; yet when I had my own practice I paid 52%; the profit margins are a no-brainer. They will then harvest the greatest possible return from the various Medical Card payments, and chronic disease schemes. They can afford to pay GPs good salaries, and hire a minimum number to do the husbandry. This type of corporate General Practice is entirely unregulated in respect of the service it provides (or doesn’t provide) for patients.
These profit driven behemoths are presumed to function in the same way as the traditional Family Doctor. For the most part they are left to their own devices, sucking up a maximum amount of HSE payments and returning a token level of care. They conceal the inadequate service behind a rigid appointment system that keeps patients waiting, the workload at sustainable level, and profit margins as high as possible.
For all their faults these centres are the inevitable future for General Practice, they are what people think they want, and what politicians are eager to give them.
To interface with this industrial model, patients must increasingly learn to translate all of their pain into the unaccommodating language of medical pathology; human beings and their emotional realities become invisible and entirely medicalised. Deeper truths behind the pain, the fear, and the anxiety that are an increasing part of everyday life for all of us, evade this more sophisticated model of Primary Care. The emergent mystery becomes just another number on another waiting list.
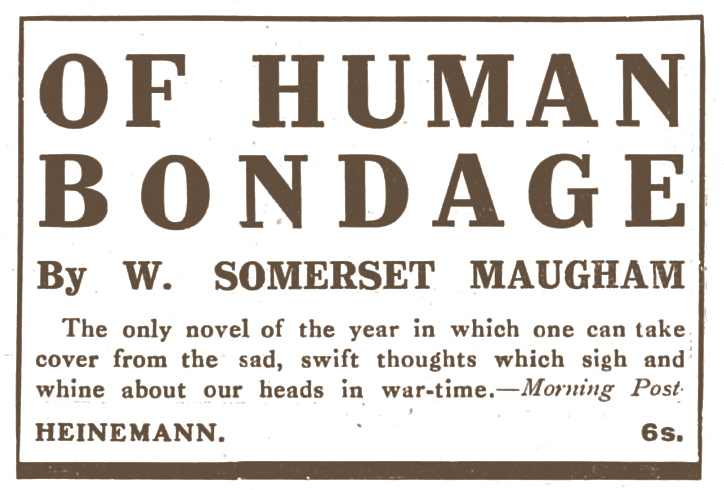
Of Human Bondage
In my early twenties after reading Somerset Maugham’s novel Of Human Bondage, I thought about becoming a Doctor. I didn’t especially want to help people, but I wanted to be in a position whereby I could help them if I wished.
I might have wanted to ‘help people’ in some vague way, but I wanted to help myself first. For a time I probably translated this notion into the more noble expression that many of my colleagues prefer to cling to. It is refreshing to hear honest medical motives expressed in the more acceptable language of a ‘work life balance’.
Maugham’s novel is about all kinds of bondage, the one I wished to liberate myself from was poverty. Medicine has at least afforded me that compensation for the small price of my soul and at times my sanity. I never imagined that I would come to see the career itself as a kind of bondage; a darkening cave wherein we can no longer see the chains or the flickering shadows on the wall.
Many Doctors know there is no need for the antibiotic, no need for the hospital referral, the scope or the scan, and yet we increasingly act according to our own benefit, or that of our employers. Convenience and fear of complaint are the other silent incentives.
In Ireland and abroad, private obstetric care is more likely to result in a caesarean section, and a child with private health insurance is more likely to end up with grommets or a tonsillectomy. Medicine has always been an uncomfortable marriage between profit and compassion. Lately it seems that profit has separated, and is suing for divorce as well as damages.

Image Daniele Idini.
Hope Deferred?
Perhaps the only thing worth saving in General Practice – the most beautiful and essential thing – is the thing that has almost disappeared; the unique nature of the relationship between the family Doctor and the families who attend him or her.
That ‘thing’ is something many people may have once enjoyed and may still enjoy with some ‘old-fashioned’ GPs. It is the thing that saved many lives during the Pandemic, more so than; masks, vaccines or spending ten euro on a pint and a sandwich.
Any future validity for General Practice would be contingent upon training GPs properly, educating them (and patients) to participate in that old partnership in an honest and meaningful way. For the moment however, the relationship is broken. The modern GP is not trusted in the manner that the family doctor once was, and he is wary of his patients or views them solely as a means to a private end. The problem is a million light years away from medical schools, training bodies or public health campaigns, all of whom have their heads in the trough.
Before former Health Minister Mary Harney reformed the Medical Council in 2007, into a weapon for the indignant and a cosy club for political appointments; the family doctor might have been a man or woman with an honest opinion in respect of your health.
An opinion that you could take or leave as you saw fit. Presently, Doctors are not trained to be honest or even candid with patients, quite the contrary in fact. Candidness was something that was permitted years ago. Often (but not always), it was a good and a welcome kind of honesty. The GP had the ‘power’ to tell you that you were ‘too fat’, ‘overly anxious’ or that you didn’t need to be immediately referred for a battery of tests or scans on demand. The GP was frank, candid and honest, and was even expected to be so. Some Doctors and GPs were lazy in their old-fashioned power, and things were sometimes missed, like cancers and physical disease. People were sometimes abused with insensitive words or beaten with the religious paradigm of the day.
Today it is increasingly rare (if not impossible) to encounter a GP who would be willing to run the gauntlet of refusing a test or having a frank conversation with the newly emancipated patient turned consumer. Training bodies and the Medical Council indirectly insist upon an obsequious dishonesty as the gold standard. They advise Doctors to give ‘back pocket’ prescriptions, a euphemism for the unnecessary antibiotic on demand. Happy customers are presumed to equate with healthy patients. The universal goal is a consumer, pleased with the product they have purchased, or recently become entitled to.
A GP might be sanctioned for using the word ‘fat’ inappropriately, and yet he or she will be rewarded in various ways should he provide an inappropriate prescription for a trendy weight loss injection; a diabetic drug currently in short supply as it is being over prescribed in the community for cosmetic purposes.
As an institution, General Practice thrives upon; ignorance, compliance and government subsidy. Most consultations in primary care amount to a waste of time in respect of public health or genuine pathology. An increasing majority attend the GP simply because they have to, or because they have been encouraged or allowed themselves to become prescription drug addicts.
Sometimes, disease becomes an identity; a form of socially sanctioned escape from an unpleasant and painful life. Illness is very often the veil that is worn to conceal a deeper unhappiness. Often, chronic illness becomes a persona with a social and financial incentive, one that can be as alluring and addictive as any drug.
In my own experience far too many ‘sick’ people are simply very unhappy. General Practice in its current form is utterly ill-equipped to deal with, or even to recognise the unhappiness or anxiety that is its principal presentation.
Increasingly, during my years in clinical practice, I found that telling a patient that they are ‘normal’ or that they have ‘normal results’ can cause a kind of disappointment. For some people, telling them they are normal is like denying their pain, barring them from Kafka’s Castle, refusing them a diagnosis and an entry into the legitimate world of the sick.

Image: Daniele Idini
To Italy
“Are you the farmer? We’ve gone on holiday by mistake!”
‘Withnail and I’
In many countries the expensive appendage of General Practice has already disappeared. Outside of the catchment area of ‘old victorian ways’, one attends an accident-clinic in the event of an accident, and almost everything else is self-referred to a specialist; a hospital consultant with rooms in the nearby town or city.
In places like Northern Italy, the Middle East, the U.S. and many more, people do not need a magic letter from a GP to get to see a ‘real doctor’. One simply makes an appointment at the consultant clinic, the receptionist will assign the headache to the neurologist, or the gastritis to the gastroenterologist and so on. Sick children are brought to see paediatricians, those wishing to become more beautiful attend the plastic/cosmetic surgeon, and old people are brought to see a geriatrician before being dropped off at the nursing home. Friendly secretaries will triage and normally arrange a bed over the phone. The first consultation usually occurs with the patient in a bed on the hospital ward. The bill is sent to the state or the insurer.
I am not suggesting for a moment that this is a better system, it is a system that was the principal cause of the horrific scenes in Lombardy during the Pandemic. Covid killed too many elderly people, that much is true, but it was the condition and organisation of the Italian health service in Northern Italy that allowed Covid to become the catastrophe that dominated the television networks.
If we think about it, cholera and a few other diseases (rather than starvation) were responsible for half of all the deaths during the Irish Famine (1847-1851). Now, imagine the hue and cry that would emerge if some renowned British Epidemiologist tried to suggest that half of the total number of Famine victims did not die of the Famine, but died instead from a coincidental ‘pandemic’ of Asiatic Cholera? What remains of the IRA would undoubtedly issue a fatwa.
Apparently when it comes to the Great Famine, we are quite capable of recognising that social conditions (poverty/famine) created the environment where disease festered and then killed exponentially. We don’t blame Cholera for the Famine, we blame the famine for Cholera. It was the Famine that created the conditions for Cholera to thrive, and it was English policy that created the conditions for the Famine itself.
Equally, the Covid virus was not the principal cause of the terrible scenes in Northern Italy. It was the absence of community medicine that created the conditions necessary for the tragedy to unfold in the horrific manner that it did.
There is, and was, no system of community medicine throughout much of Northern Italy when Covid arrived. In Lombardy; frail, elderly people with Covid, had no one to call, other than consultants and specialists, who then flooded their hospitals with Covid and transformed them into the geriatric hotbeds of disease and mortality that provided the horror show, and fuelled the fear-frenzy. That same frenzy soon transformed Covid from a cohort specific disease, into a pandemic that requires universal vaccination, lockdowns and allegedly kills almost everyone it touches.
At home the Italian mistakes were coarsely imitated by the Irish Government as they cleared the public hospitals and transferred a mass of untested, convalescing hospital patients, into all available beds in the Nursing Homes. They introduced Covid into the sector en masse, firmly and strictly locked it in, and thereby caused (or at least facilitated) a wave of death that has yet to be investigated.
The truth about Italy was opined in an article that appeared in the NYT in November 2020 entitled ‘Why Covid Caused Such Suffering in Italy’s Wealthiest Region’.
In 2016, Lombardy — home to more than 10 million people — saw only 90 medical school graduates go on to pursue specialised studies toward becoming general practitioners. They received annual scholarships of 11,000 euros (nearly $13,000), less than half those secured by people preparing for specialties like cardiology. The numbers have grown in recent years, but not enough to replace retiring general practitioners, medical associations say.
The point I am making here, is that despite the fact that General Practice might well be an overall pathology in Ireland; that is not to say that the institution does not accomplish some purely accidental good. A broken clock will tell the right time twice a day.
Many Irish lives were inadvertently saved by the fact that patients had a relationship with a Doctor (their Family Doctor). One whom they could call and who would tell them what they should or should not do.
Despite the fact that medical advice from the oracle of General Practice amounted to little more than: ‘stay at home and suffer on’; it was the simple fact of having a relationship with a contactable GP that reassured and ultimately saved lives.
Needless to say, (proportionally at least) far more lives were saved by GPs like Dr Pat Morrissey in Adare, and several others – some of whom who became part of a covert network who insisted (despite threats from the IMC president) upon doing more for very sick patients – than simply telling them to ‘stay at home until they turned blue’.
Public health officials were quick to see the value of this old-relationship and offered GPs an unvouched blank cheque, to the tune of €30 per reassuring phone call. However, beyond a phone consultation, Irish GPs by and large did not provide any interventional ‘care’ for those whom they advised to ‘stay at home’.
Nonetheless they saved lives and avoided an Italian-type tragedy simply because those lives had access to a Doctor within their own community. During Covid, it did not matter if GPs were wilfully useless; it only mattered that people had access by phone, by video-link or smoke signal. They were not entirely alone.
The miracle of science was with them, and they stayed in the safest place, far away from established medicine. Whilst Covid patients were in contact with their GP, they were cared for at home by their families. This was not the case in Northern Italy where even a token degree of Community Medicine was non-existent. A passage from the NYT article states the following:
When the first wave hit, Milan — a city of more than 1.3 million — had only five doctors expert in public health and hygiene, said Roberto Carlo Rossi, president of Milan’s Doctors’ and Dentists’ Guild. They were responsible for setting up a testing and contact tracing regimen.
Where most Irish GPs did in fact care for patients in practical terms, was in the Nursing Home. We were the responsible physicians and were the only ones allowed in.
As a consequence of our careless ‘care’, combined with political ineptitude; over a thousand died alone, and in truly horrible conditions, all within a matter of months. During that time Covid payments in respect of their care were doubled, trebled and quadrupled, in spite of the death rate and the abject failure to deliver what might be described (in third world terminology) as ‘the very basics’.
The survival of honest medicine may depend upon an old-fashioned relationship with a different type of Doctor. One who is often found to be ‘non-compliant’ at Medical Council Hearings. Yet, to paraphrase an old philosopher: ‘there may be a different court, one that is higher than the Courts of men; one where a great many of the judgements of this world, will doubtlessly be overturned.’