Déjà Vu
As Covid-19 sweeps through Ireland, I can’t help experiencing a feeling of déjà vu. In early 2015, I was based in Guinea as part of the international response to the Ebola epidemic ravaging west Africa. I was responsible for reporting on the progress of the epidemic as well as the measures being applied to halt its further progression. An important element of my work was in helping define the potential recovery needs of the country and articulating a vision as to how the international agency I was working for could contribute in helping Guinea transition from the ongoing short-term emergency humanitarian focus to a middle-long term recovery and development operational approach.
Conakry in the Time of Ebola
Prior to travelling to Guinea, I had read everything I could find both about Ebola and the situation on the ground. Similar to Covid-19, Ebola is a virus and is also believed to originate from bats. However, it is far more virulent, can result in serious haemorrhaging with severe internal and external bleeding and has a far higher death rate.[i] The first Ebola case in west Africa occurred in late December 2013 in Guinea. A 2 year-old boy in the village of Melandiou, close to the Guinean border with Liberia and Sierra Leone feel ill with a mysterious disease, later identified as Ebola and died a couple of days later.[ii] His grandmother, pregnant mother and three year old sister died shortly after.[iii] Ebola was on the march.
In the latter half of 2014 and early 2015, the media was full of apocalyptic descriptions and assessments of the impacts of Ebola on Guinea, as well as its neighbours Liberia and Sierra Leone, and the danger of its spreading further afield. However, the situation on the ground in Conakry which greeted me upon my arrival, was not at all what I had expected. If I had not been aware of the virulence and mortality rate of those who contracted Ebola, I could easily have been convinced that its threat had been seriously over-hyped.
While hand sanitisers were omnipresent and my temperature was taken each time upon arrival at the office, as well as when visiting other organisations, there appeared to be little restriction on the movement of people in Conakry. There was an abundance of economic activity as people moved freely through the streets and the colourful markets heavied with custom. Street food vendors displayed and sold their succulent delicacies to eager passers-by. Aspiring footballers practised their skills on the open roads, briefly making way for passing traffic, while others jogged through the streets. One bridge I passed, several times a day, had a perpetual presence of primarily young men performing their workouts and practising stretches from early in the morning until late evening. A sofa conveniently placed at the end of the street, where our office was located, had been drafted into service as a temporary meeting place for an ever-changing guard of young males.

Conakry in the time of Ebola. (c) Justin Frewen
The absence of constraints on physical proximity was particularly evident during the finals of the African football Cup, for which Guinea had qualified after a long absence. In the days leading up to the tournament, a tangible thrill of expectation hung in the air as pockets of people congressed in the streets and cafes to assess their country’s chances. The day of the tournament launch, a pair of enormous speakers were placed in the street behind our office. From 8 AM onwards, music blasted through the neighbourhood. From my vantage point on the second floor, I could see boys and girls dancing in their gardens and passers-by congregating to animatedly discuss the imminent tournament kick-off. A middle-aged woman walked down the street laden with two substantial shopping bags. As she neared the source of the pulsating beat, a broad smile flickered across her pleasant features as she swayed to the rhythm without missing a stride. Some 20 metres later, she resumed her erstwhile gait and homeward struggle with her sagging shopping bags.

International Women’s Day, Conakry,, Guinea, Justin Frewen.
Coronavirus Lockdowns
In contrast, the current coronavirus pandemic has led to lockdowns of varying intensities around the world. As early as 24 March, the Guardian newspaper highlighted how some 20% of the world’s population was under lockdown imposed as a result of Covid-19.[iv] The past month, if anything, has seen a radical increase in the imposition of such measures and the consequent reduction of social and economic activities to prevent the onward transmission of this virus. This contrasts sharply with the general situation in Guinea during the Ebola crisis. Although strict quarantine was imposed on those who contracted Ebola and in spite of the lurid accounts of Ebola’s impact upon the people of Guinea, Liberia and Sierra Leone, there was paradoxically far less overt evidence of its threat in daily, public life.
The primary reason for this difference lies in the transmissibility of the respective viruses that lead to Ebola and Covid-19. As outlined by ‘Médecins sans frontières’ (MSF – Doctors Without Borders), who were instrumental in rallying international awareness and required resources to tackle Ebola, “(H)uman to human transmission occurs through contact with bodily fluids of an infected person or through surfaces contaminated with these fluids.”[v] Covid-19, like other common human coronaviruses, transmits from an infected person a) in water droplets through the air, as a result of coughing or sneezing; b) close personal contact such as shaking hands; and c) touching one’s face (eyes, nose, mouth) after touching an object / surface before washing one’s hands.[vi]
It is therefore clear the potential onward transmission of Covid-19 is far greater than for Ebola, as it does not require direct physical contact with the carrier of the virus. Fortunately, it appears that it cannot be transmitted through the air directly which would greatly increase its range and ease of transmission.[vii] This fact has led to a far greater restriction on social and economic life due to Covid-19’s enhanced transmissibility that was the case with Ebola.
Virus Mobility
Ebola’s infection spread was relatively localised. Despite the occurrence of a few cases outside the epicentre of west Africa (Guinea, Sierra Leone and Liberia), such as in Scotland and North America predominantly via the return of health workers, the virus was effectively contained. Approximately 11,000 people succumbed to the illness and while each of these fatalities was a tragedy for the victims and their loved ones, this figure obviously pales in significance to the rapidly increasing daily totals of Covid-19. As I write today, on 24 April, the recorded deaths are fast approaching 200,000. These figures, however, are undoubtedly a significant underestimation of the actual number of people who have succumbed directly to this coronavirus, not to mention those who may have succumbed to secondary infections due to enfeebled immune systems. In the UK, for example, the daily figures of deaths released to the public do not include those that have occurred in nursing homes or other residential settings.[viii]
One of the major issues confronting health personnel combating Ebola in Guinea was the mobility of people in this region as there was widescale migration by people particularly in the rural areas to obtain income for their families. This situation was aggravated by the porous frontiers between neighbouring countries as people would often traverse national borders in search of work and food or even simply to visit their extended family. Borders in Africa have frequently been subject of fierce contestation and the manner in which they were imposed during colonialism has been one of its most enduring, negative legacies. They have both divided members of ethnic groups, as in the case of the nomadic Tuareg of North Africa, and also forced members of diverse cultural and religious groups into a single polity, such as the Sudan or Nigeria.
In tackling Ebola, it became clear that the presence of these different national jurisdictions, divided by arbitrary and highly porous borders, such as those that existed between Guinea, Sierra Leone and Liberia greatly complicated the tracing of potential contacts of Ebola victims. Frequently, there would be no accurate records of who had crossed from one country to its neighbour. During the Ebola epidemic this resulted in severe delays in tracing potential contacts of Ebola victims, with the potential that these contacts could inadvertently become the source of waves of new infections as they moved from one place to the next.
While Ebola was spread in west Africa predominantly through the movement of local people in rural areas trying to augment their meagre incomes, the worldwide dissemination of Covid-19 has been by the more relatively globally affluent. The massive growth in air travel has greatly increased the ease by which viruses can move from one part of the globe to another via their human hosts. When the Spanish Flu, so named because the flu was first widely reported on there, global movement was far slower and it therefore took the virus far longer to journey from one region to another. Today, we can get to virtually anywhere in the world in under 36 hours. This makes it far more difficult to control the onward progression of viruses such as Covid-19 and to effectively localise their impact, as was the case with Ebola.[ix] It should be noted that this risk had been noted as an issue of concern prior to the current pandemic.[x]

‘The massive growth in air travel has greatly increased the ease by which viruses can move’
Fear and ‘loathing’
A frequent occurrence in serious epidemics and pandemics is the parallel transmission of fear which can radiate through impacted communities, even amongst those not yet exposed to the pathogen. A particularly tragic episode during the Ebola crisis occurred in September 2014 in the southern Guinea village of Wome when a team of eight health workers and journalists were murdered. The villagers were terrified that this deputation, which had been sent to help there and fearing they were there to spread the disease, attacked them violently with clubs and machetes.
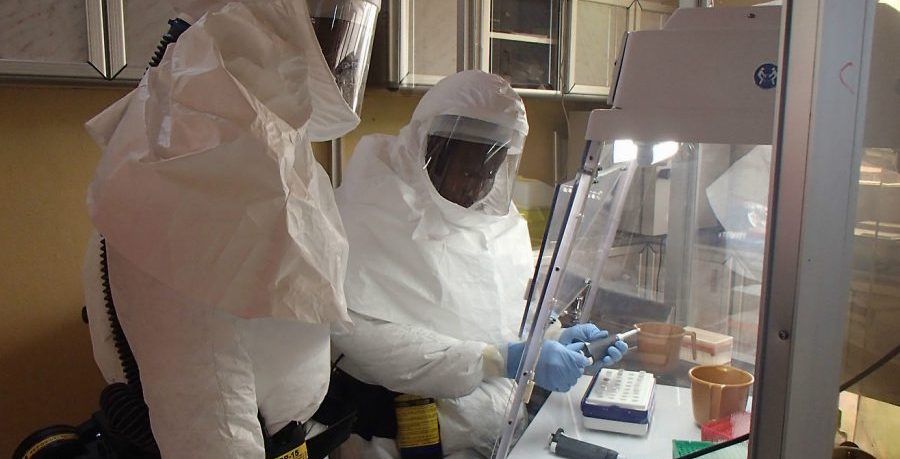
Although unique in terms of loss of life, the tragedy at Wome was not an isolated event. The Red Cross reported that its teams were attacked an average of 10 times per month over a year by frightened members of the local population.[xi] While there was a degree of understanding amongst member of the international community in Guinea as to the apprehension of local people confronted by outsiders, particularly those decked out in full hazmat suits, there was also disbelief that this could result in such aggression. Outside Guinea, people generally express incredulity at what transpired at Wome. How could people be so ill informed or be in such a state of fear that they would murder those sent to provide assistance. This would surely never happen in ‘developed countries’.
However, if there is one thing we have learnt from Covid-19, it is that the people of Wome were in no way exceptional in falling victim to the plague of fake rumours, conspiracy theories or the negative treatment of health personnel.
Over the Easter weekend in England, numerous phone masts were set on fire amid claims they were spreading the coronavirus. In the early hours of April 14 in Huddersfield, dozens of people had to be evacuated from their homes as a nearby phone mast was set ablaze.[xii] Similar fires were also reported earlier in April at masts in Birmingham, Liverpool and Melling in Merseyside. A video was shared on Facebook and YouTube, allegedly documenting a fire in Aigburth while claiming a link between Covid-19 and mobile technology.[xiii]
One such attack also impacted directly upon the victims of coronavirus when, in Birmingham, a phone mast serving the NHS Nightingale Hospital was targeted by arsonists.[xiv] Mobile masts have also been set alight in Ireland with the latest incident occurring in Cork on the night of 22 April.[xv] Rumours linking Covid-19 and 5G technology have been spread by social media sites such as Facebook, YouTube and WhatsApp, leading to questions as to whether greater control should be exercised over these media to which their providers have responded by deleting what they categorise as false or harmful content related to the virus.[xvi] Intriguingly, there have been reports that social media has also been used in some places to name and shame people breaking social movement restrictions in their communities.[xvii]
There has been deserved widespread praise for those on the frontline of the fight against Covid-19, including nightly clapping by the general public to display their support of health workers. Starting in Italy and Spain, this tribute has spread to many countries around the world. Despite these public accolades, health professionals have been abused in public on account of their engagement in tackling coronavirus. While these incidents have not resulted in fatalities, as in Guinea, they have been extremely disturbing. In early April, Howard Catton, CEO of the International Council of Nurses, revealed his organisation had received reports from around the world of abuse and harassment related to their work in fighting Covid-19. According to Catton, nurses were seen as potential carriers of the virus and thus a threat to the communities in which they lived.[xviii] In England, nurses have been abused in public and accused of being disease spreaders.[xix] Heath personnel have even been forced to quit their accommodation by landlords afraid they may contract the virus from them. In one such instance, Joseph Alsousou, a surgeon based in Oxford was asked to leave his rented accommodation as soon as possible.[xx]

Health Care workers.
From Ebola to Covid-19: Has the WHO Failed Again?
The WHO came under severe criticism for its handling of the Ebola epidemic. The international president of Médicins Sans Frontieres (MSF), Joanne Liu, appeared before the UN Security Council in September 2014 to inform the members directly as to how Ebola was impacting upon west Africa. She revealed that MSF was effectively engaged in building “crematoria instead of hospitals”. The same month Liu demanded that UN members deploy civilian and military resources to tackle this emergency.[xxi]
Following the successful containment of the Ebola outbreak, the WHO apologised for its failure to respond in time and promised to undertake the necessary reforms to avoid a similar situation in the future. However, less than five years later, the WHO is once again under attack for its alleged slowness to respond to the outbreak of Covid-19 and its delay in communicating the gravity of this outbreak to the world at large. To punish the WHO the U.S. President Donald Trump has announced he will withhold the U.S. contribution of US$400 million to the WHO.[xxii] Although some commentators have pointed out that in fact the figure of $400 million is an overestimation given that the U.S. is already as much as $200 million behind in its pledged contributions,[xxiii] this has the potential to seriously disrupt WHO operations at this critical moment.
In effect, while there are understandable concerns that the WHO could have reacted more promptly and effectively to the outbreak of Covid-19, this is not the time to engage in such an analysis. As its Director-General has stated the WHO’s performance in tackling this pandemic will be reviewed both by member states and independent bodies to identify failures in the organisation’s performance.[xxiv] The ongoing underfunding of the WHO together with the organizations endemic internal problems, which predated this crisis, will hopefully feature in this review.[xxv]

WHO Headquarters in Geneva, Switzerland.
Clear Communication
As illustrated in contexts as diverse as New Zealand and Kerala, successfully tackling Covid-19 requires a communications strategy that provides clear guidelines and recommendations, supported by transparent explanations as to the approach adopted through easily accessible media platforms. In Kerala, the state government provided detailed media briefings on a daily basis outlining the necessary actions to tackle the virus, the importance of contact tracing, the need for quarantining and training for healthcare and hospital personal while also seeking the support and cooperation of the general public in surveillance and containment.[xxvi] These daily briefings proved highly popular and earned widespread public respect for the manner in which decisions and their rationale were explained. Updates on government actions to tackle the virus, relayed through the Chief Minister’s social media accounts, also proved highly popular. The effectiveness and accessibility of these communication measures resulted in a statewide awareness of Covid-19 and the necessity for close cooperation and mutual support between the health service and public to reduce transmissibility and avoid clinical case overload.[xxvii]
In addition to providing Covid-19 related information through standard media channels, the NZ Prime Minister, Jacinda Ardern, has communicated directly with the public, making herself available to the media and holding daily public press conferences, led by New Zealand’s director-general of health, Dr Ashley Bloomfield. Together they have displayed “a reliable, measured and authoritative face for New Zealand’s Covid-19 response”. [xxviii] Of particular value has been the clarity of Jacinda Ardern’s communication on the virus.[xxix] Her leadership style has been assessed by one commentator as “one of empathy in a crisis that tempts people to fend for themselves. Her messages are clear, consistent, and somehow simultaneously sobering and soothing. And her approach isn’t just resonating with her people on an emotional level. It is also working remarkably well.”[xxx]

Jacinda Ardern, New Zealand’s Prime Minister.
Uncharted Territory?
One of the primary excuses offered for the difficulty in responding to Covid-19, has been that it is unprecedented and there is no reliable roadmap to guide us. However, while the current situation whereby so many countries have implemented lockdowns of varying levels of severity, closing down large sectors of their economies, is unique, it would be false to argue that we had no warning of the possibility of such an event.
The first two decades of this millennium has been witness to several new epidemics, that could potentially have had a similar, if not far worse, outcome than Covid-19. Two of these were also coronaviruses, namely Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS). In 2002, SARS originated in Hong Kong, resulting in 8,098 reported cases and 774 deaths, a mortality rate of just under 10%.[xxxi] Middle East Respiratory Syndrome (MERS) was first identified in Saudi Arabia in 2012 and spread to several countries. By the end of November 2019 some 34.4% of patients infected by MERS-Cov had died (858 of 2,494 laboratory confirmed cases).[xxxii] In 2014, Ebola first struck west Africa. Although mainly contained to Guinea, Liberia and Sierra Leone, there were a number of cases in other countries. In 2018, another outbreak of Ebola occurred in the Democratic Republic of Congo (DRC), the 10th in 40 years. As of 19 April 2020, there had been 3,316 confirmed cases, resulting in 2,277 deaths or a mortality rate of almost 69%.[xxxiii]
Many warnings have also been given by experts that a significant threat of a pandemic existed.[xxxiv] There has been at the very least an awareness that the threat of a pandemic which could result in significant fatalities and international disruption existed. Several countries had undertaken simulations that pointed out where major risks lay in terms of their readiness to counter such a threat. The US alone has held several of these exercises since the turn of the century, which had pointed out severe deficiencies in its preparedness.[xxxv]
Kerala – a model to tackle Covid-19?
The southern Indian state of Kerala which has been widely praised for its response to Covid-19. Its success would appear to be based upon two major elements. The first was the speed with which the state reacted to its outbreak in Wuhan. The health minister, K. K. Shailaja, alarmed by news of the virus in China and aware many students from Kerala were studying in Wuhan, organised a high-level meeting to discuss the situation on January 25th. The following day a control room was established to coordinate the department’s work. Eighteen committees were established and held daily meetings to evaluate actions undertaken and host daily conferences where Shailaja briefed on the actions her department was undertaking. The slogan “Break the Chain” has been given to the approach adopted in Kerala where open quote contact tracing” is implemented. This involves tracing all who have potentially been in contact with the infected person, similar to that approach which was critical in tackling Ebola.
By March 19, Kerala had 25 people who had tested positive and 31,173 people under surveillance, of which 273 were isolated in hospitals with the rest quarantining at home. These high numbers were mainly due to the high influx of travellers, including people from Kerala returning home. On March 18 and 19 alone, 7,861 and 6,103 people respectively were put under surveillance. The resources required, both in terms of management and coordination as well as the active input of all sectors of society, leads to the second reason why Kerala has proved so successful to date in its struggle against Covid-19.
The second critical element in Kerala’s approach is the existence of a strongly supported and well-funded public health sector, which forms a strong health shield against epidemics and other threats, even in a state which would be relatively poor compared with Europe and the U.S. This has been greatly supported by the active participation of a strong grassroots section of the state’s public which has combined with the health service to fight Covid-19. [xxxvi]
When one contrasts the resolute measures, large scale mobilisation and effective containment of Covid-19 by a state such as Kerala or a nation like Vietnam – a country of over 96 million people, which despite sharing a border with China had only 268 cases and no fatalities as of 24 April – one cannot but be impressed at their performance. By the same token, one has to question how these relatively resource poor polities have been able to handle this crisis so much better, at least up to now, than the affluent nations in Europe and the U.S..

The Indian state of Kerala has been widely praised for its response.
What Lies Ahead?
While it is difficult, at this stage, to estimate with any certainty the actual mortality rate of this coronavirus, it is certainly far less lethal than Ebola. Although Covid-19 discriminates greatly against the elderly in our society, its mortality rate is probably inferior to 1% and is likely to be less than this. However, whether we will ever be able to effectively assess the actual number of Covid-19 cases and related deaths is itself a moot point given the wildly varying rates of testing for the virus in different countries, the differing methods for compiling statistics related to deaths and the fact that almost certainly many deaths that occur as a result of this virus will never be acknowledged.
Moreover, there is still much we do not know about this coronavirus. For example, do those who contract and survive Covid-19 gain immunity and, if so, would this be short or long-term? In South Korea, people who appeared to have recovered have later tested positive again for the virus, though preliminary Indications are that rather than being reinfected, the virus has been reactivated.[xxxvii] Similarly in China, patients who had apparently recovered from the virus are still registering as positive without displaying any symptoms. One 50-year-old man was still testing positive some two months after he first acquired Covid-19.[xxxviii] Given the complexities of and uncertainties related to Covid-19, the current phase consisting of lockdowns and other physical isolation measures may yet prove the easier part of our struggle to return to normality.
If the virus can remain dormant in our system with the possibility of being reactivated and/or being transmitted onwards, the struggle to eradicate Covid-19 becomes infinitely more complex. Either coronavirus victims who continue to test positive, despite not displaying any symptoms, might require extended periods of isolation until they are no longer considered potential vectors of onward transmission or there is an approved vaccine in place. The earliest estimate for such a vaccine, despite acceleration of the testing process worldwide, is mid-2021. However, we need to remember there are still no vaccines for the four coronaviruses, including SARS and MERS, that currently circulate amongst humans.[xxxix]
Certainly, the spread of Covid-19 has been far more extensive than Ebola. However, its transmission rate is only one of the issues facing us today. Just as certain underlying health conditions – cardiovascular disease, cancer, diabetes, high blood pressure – can severely aggravate the impact of coronavirus, this coronavirus could have widespread knock-on effects even more deleterious than its health impact. Covid-19 could become an underlying condition, which will lead to serious economic and social disruption as a result of measures applied to counter its spread. We have even been warned that we could face a worse depression that that which provoked by the Wall Street crash of 1929.[xl]
A further significant area of concern is that of food supply. Although supermarket shelves in the global North, despite earlier panic buying, have been kept sufficiently stocked for our immediate needs, this may not last. Should this pandemic continue for an extended period of time, food supply chains will almost certainly be weakened, if not effectively broken. Food chains are complex structures, composed of intricate, interlinked and interrelated elements – agricultural producers and inputs, large brokerage agencies, shipping and land transport companies and distribution nodes, which are all subject to potential disruption. According to the Food and Agricultural Organization (FAO), reported shipping industry slowdowns due to foreclosures and logistic blockages could soon start to disrupt this chain.[xli] The consequences for the Global South could be catastrophic with potentially hundreds of millions threatened by food insecurity.[xlii]
In short, when and how will the global economy recover? As an article on the McKinsey site bluntly puts it, “(T)he pandemic’s economic challenges are unprecedented.”[xliii]
[i] World Health Organization (WHO), Ebola virus disease, WHO, accessed 24 April 2020, https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease
[ii] WHO, Ground zero in Guinea: the Ebola outbreak smoulders – undetected – for more than 3 months, WHO, accessed 24 April 2020, https://www.who.int/csr/disease/ebola/ebola-6-months/guinea/en/
[iii] Dr. Jonathan D. Quick, The End of Epidemics: The Looming Threat to Humanity and How to Stop it, Scribe Publications, Brunswick (Victoria) Australia / London U.K., p. 27
[iv] Davidson, Helen, Around 20% of global population under coronavirus lockdown, Guardian, 24 March 2020, https://www.theguardian.com/world/2020/mar/24/nearly-20-of-global-population-under-coronavirus-lockdown
[v] MSF, Ebola and Marburg: Quick Facts, MSF, accessed 23 April 2020, https://www.msf.org/ebola c
[vi] Centers for Disease Control and Prevention (CDC), Common Human Coronaviruses, CDC, accessed 23 April 2020, https://www.cdc.gov/coronavirus/general-information.html
[vii] World Health Organization (WHO), Q & A on coronaviruses (Covid-19), WHO, accessed 23 April 2020, https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
[viii] Chris Giles, UK coronavirus deaths more than double official figure, according to FT study, Financial Times, 22 April 2020, https://www.ft.com/content/67e6a4ee-3d05-43bc-ba03-e239799fa6ab; Niamh McIntyre & Pamela Duncan, Care homes and coronavirus: why we don’t know the true UK death toll: Government figures only tell part of the story as they only cover hospital deaths, 14 April 2020, https://www.theguardian.com/world/2020/apr/14/care-homes-coronavirus-why-we-dont-know-true-uk-death-toll
[ix] Geoffrey Holland, COVID-19, and Pandemics on a Crowded Planet – A MAHB Dialogue with Infectious Disease Expert, Arthur Reingold, Millennium Alliance for Humanity and the Biosphere (MAHB), 12 March 2020, https://mahb.stanford.edu/blog/covid-19-and-pandemics-on-a-crowded-planet-a-mahb-dialogue-with-infectious-disease-expert-arthur-reingold/
[x] Aidan Findlater & Isaac I. Bogoch, Human Mobility and the Global Spread of Infectious Diseases: A Focus on Air Travel, Trends in Parasitology (Vol 34, Issue 9), September 2018, https://www.cell.com/trends/parasitology/fulltext/S1471-4922(18)30142-9, pp 772-783
[xi] Dr. Jonathan D. Quick, ibid, p. 150
[xii] BBC Coronavirus Pandemic News, Huddersfield phone mast fire ‘put residents at risk’, BBC, 14 April 2020, https://www.bbc.com/news/uk-england-leeds-52279341
[xiii] BBC Coronavirus Pandemic News, Mast fire probe amid 5G coronavirus claims, BBC, 4 April 2020, https://www.bbc.com/news/uk-england-52164358
[xiv] Mark Sweney and Jim Waterson, Arsonists attack phone mast serving NHS Nightingale hospital, Guardian, 14 April 2020, https://www.theguardian.com/technology/2020/apr/14/arsonists-attack-phone-mast-serving-nhs-nightingale-hospital
[xv] Adrian Weckler, Mobile mast near Cork Apple headquarters set ablaze in suspected 5G arson attack, 23 April, https://www.independent.ie/irish-news/mobile-mast-near-cork-apple-headquarters-set-ablaze-in-suspected-5g-arson-attack-39151454.html
[xvi] BBC Technology News, YouTube bans ‘medically unsubstantiated’ content, BBC, 22 April 2020, https://www.bbc.com/news/technology-52388586
[xvii] Alice Yan, Chinese web vigilantes name and shame people for breaking coronavirus quarantine, South China Morning Post, 20 March 2020, https://www.msn.com/en-sg/news/other/chinese-web-vigilantes-name-and-shame-people-for-breaking-coronavirus-quarantine/ar-BB11tD2i
[xviii] Stephanie Nebehay, Nurses must be protected from abuse during coronavirus pandemic: WHO, nursing groups, Reuters, 6 April 2020, https://in.news.yahoo.com/nurses-must-protected-abuse-during-220640671.html
[xix] Rebecca Gilroy, Nurses of coronavirus frontline facing ‘abhorrent’ abuse from public, Nursing Times, 20 March 2020, https://www.nursingtimes.net/news/coronavirus/nurses-fighting-coronavirus-facing-abhorrent-abuse-from-public-20-03-2020/
[xx] BBC Oxford, Coronavirus: Doctor ‘kicked out’ by Headington landlady, BBC website, 25 March 2020,https://www.bbc.com/news/uk-england-oxfordshire-52032909
[xxi] Dr. Jonathan D. Quick, ibid, p. 170
[xxii] David Smith, Trump halts World Health Organization funding over coronavirus ‘failure’, The Guardian, 15 April 2020, https://www.theguardian.com/world/2020/apr/14/coronavirus-trump-halts-funding-to-world-health-organization
[xxiii] Binoy Kampark, The WHO, Trump And The Coronavirus Wars, Oriental Review, 18 April 2020, https://orientalreview.org/2020/04/18/the-who-trump-and-the-coronavirus-wars/
[xxiv] WHO, Rolling updates on coronavirus disease (Covid-19), WHO, accessed 24 April 2020, https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
[xxv] Linton Besser, World Health Organization division tackling coronavirus underfunded and facing internal corruption allegations, audits reveal, Australian Broadcasting Corporation, 16 February 2020, https://www.abc.net.au/news/2020-02-17/coronavirus-who-underfunded-internal-corruption-allegations/11970382
[xxvi] R. Krishnakumar, Kerala model, The Hindu (Frontline series), 10 April 2020, https://frontline.thehin, du.com/cover-story/article31130309.ece
[xxvii] R. Krishnakumar, ibid
[xxviii] Bryce Edwards, Ardern has shone in the coronavirus crisis but a recession could still doom her re-election chances, The Guardian, 18 March 2020, https://www.theguardian.com/world/2020/mar/19/ardern-has-shone-in-the-coronavirus-crisis-but-a-recession-could-still-doom-her-re-election-chances
[xxix] Sam Clench, Clarity is the quality that makes Jacinda Ardern so effective in a crisis, new.com.au, 27 March 2020, https://www.news.com.au/lifestyle/health/health-problems/coronavirus-clarity-is-the-quality-that-makes-jacinda-ardern-so-effective-in-a-crisis/news-story/efbb0fcc2f80f12e83719c4f2428f5b5
[xxx] Uri Friedman, New Zealand’s Prime Minister may be the most effective leader on the planet, The Atlantic, 19 April 2020, https://www.theatlantic.com/politics/archive/2020/04/jacinda-ardern-new-zealand-leadership-coronavirus/610237/
[xxxi] NHS, SARS (Severe Acute Respiratory Syndrome, NHS, accessed 24 April 2020, https://www.nhs.uk/conditions/SARS/
[xxxii] WHO, Middle East respiratory syndrome coronavirus (MERS-CoV), https://www.who.int/emergencies/mers-cov/en/
[xxxiii] MSF, Ebola Crisis Update, MSF, 23 April 2020, https://www.msf.org/drc-ebola-outbreak-crisis-update
[xxxiv] Dr. Jonathan D. Quick, ibid
[xxxv] Nicola Twilley, The Terrifying Lessons of a Pandemic Simulation, The New Yorker, 1 June 2018, https://www.newyorker.com/science/elements/the-terrifying-lessons-of-a-pandemic-simulation
[xxxvi] Times of India Editorial, Kerala Shows The Way: Decades of investment in public health is helping the state control Covid-19 The Times of India, 16 April 2020, https://timesofindia.indiatimes.com/blogs/toi-editorials/kerala-shows-the-way-decades-of-investment-in-public-health-is-helping-the-state-control-covid-19/; M.K. Bhadrakumar, Kerala’s Covid Story is Hard to Replicate, NewsClick.in, 20 April 2020, https://www.newsclick.in/Kerala-Covid-Story-is-Hard-to-Replicate
[xxxvii] Yaron Steinbuch, More covered patients in South Korea are testing positive again, New York Post, https://nypost.com/2020/04/10/recovered-coronavirus-patients-in-south-korea-testing-positive-again/, 10 April 2020
[xxxviii] Brenda Goh, Recovered, almost: China’s early patients unable to shed coronavirus, Japan Times, https://www.japantimes.co.jp/news/2020/04/22/asia-pacific/china-early-patients-coronavirus/#.XqA9aW5FxPY, 22 April 2020
[xxxix] James Gallagher, Coronavirus vaccine: When will we have one?, BBC, 23 April 2020, https://www.bbc.com/news/health-51665497
[xl] Geoff Zochodne & Victor Ferreira, How bad could the coronavirus crisis get for the economy? Some point to the great depression, Financial Post, 20 March 2020, https://business.financialpost.com/news/economy/coronavirus-crisis-new-great-depression
[xli] Maximo Torero Cullen, Covid-19 and the risk to food supply chains: How to respond?, FAO, 29 March 2020, www.fao.org/3/ca8388en/CA8388EN.pdf
[xlii] Fiona Harvey, Coronavirus crisis could double number of people suffering acute hunger – UN, The Guardian, 21 April2020, https://www.theguardian.com/world/2020/apr/21/global-hunger-could-be-next-big-impact-of-coronavirus-pandemic
[xliii] Matt Craven, Mihir Mysore Shubham Singhal and Matt Wilson, Covid-19, Briefing note, April 13, 2020: our latest perspectives on the coronavirus pandemic, McKinsey, 13 April 2020, https://www.mckinsey.com/business-functions/risk/our-insights/covid-19-implications-for-business